Article
Coding Consult
Chronic kidney disease
If you haven't yet done so, be sure to change your charge sheet to reflect the new ICD-9-CM codes for chronic kidney disease that took effect Oct. 1. You should add seven new kidney disease codes and revise fifth-digit subclassifications in hypertensive heart and kidney disease codes.
Report CKD in stages
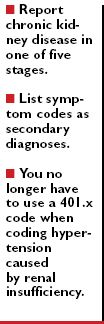
The 585 category's fourth digits simply specify in chronological order the five CKD stages from least severe (stage I) to greatest (stage V). For example, if the patient has stage III CKD, you'd use 585.3.
The new codes are:
Coding a CKD visit
When you order tests to get the patient's GFR to help determine the CKD stage, you'll need to report the appropriate E&M code (99201-99215) or lab code (if your office has a certified lab), in addition to 585.1-585.5. Otherwise, you may not be reimbursed for these tests.
For instance, say a patient presents with possible CKD. You document the medical history and perform the exam. Then, to check the GFR, you order blood creatinine (82565) and urine protein tests (84156, protein, total, except by refractometry; urine). Based on the history, exam, and test results, you diagnose stage I CKD. For the tests, history, decision-making, and exam, you report 99213 (office or other outpatient visit . . . established patient . . .) along with 585.1 as the primary diagnosis. Remember that you can list symptom codes, such as diabetes (250.xx), as secondary diagnoses.
Because the 585.x codes have dropped "chronic renal failure" in the descriptor, your documentation should specify CKD rather than imprecise terms, such as chronic renal failure and chronic renal insufficiency. CMS deleted renal failure because many kidney patients suffer from associated diseases, such as hypertension (401.x), and haven't advanced into the organ failure state, Conklin says.




