Article
Legal risks of giving information
Malpractice Consult
Mrs. A told Dr. B., "John won't tell me anything about your examination last week. I'm his wife and I have a right to know."
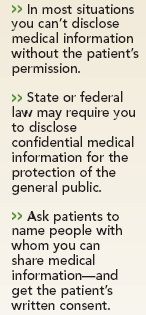
There are exceptions, though. Physicians may be required by state or federal law to disclose confidential medical information to health agencies for the protection of the general public or other individuals. For example, state law may mandate that physicians report episodes of loss of consciousness to the motor vehicle bureau. And some states require physicians to disclose a patient's direct threat of harm to another person.
To protect yourself before such situations arise, ask patients to identify individuals with whom you can share medical information as needed. Obtain the patient's written consent, and place that in a prominent and accessible section of the chart.
If a spouse or other relative routinely accompanies the patient to office visits and is permitted by the patient to be in the exam room, consent for sharing the patient's medical information might be inferred. But it's still wise to ask for and document the patient's consent.
Ask patients scheduled for surgery to identify one person with whom the surgeon has permission to talk immediately following the surgery. Ask, too, if this authorization extends to future conversations without further patient approval.
Members of your staff should also be familiar with current state and federal confidentiality laws. They should know what type of information they can and can't give out on the telephone, even to other physicians, without proper authorization.
Contact your professional liability insurer or a health law attorney when questions arise concerning the confidential medical information of minors (including a noncustodial parent's right to know) and when the law requires disclosure of confidential medical information to governmental or health agencies.
Penalties for unauthorized disclosure depend on the circumstances, but even if the effects of inadvertent revelation are minor, defending a lawsuit can be costly, so insurers are anxious to settle before trial. And legal suits aren't the only consequence. The patient also may ask the licensing board to penalize you for an ethical breach. At the least, inappropriate disclosure could disrupt the doctor-patient relationship.

The author is a risk management and loss prevention consultant in Cloverdale, CA. He can be reached by e-mail at lossprevention@earthlink.net
.
This department deals with questions on common professional liability issues. We cannot, however, offer specific legal advice. If you have a general question or a topic you'd like to see covered here, please send it to Malpractice Consult, Medical Economics, 123 Tice Blvd., Suite 300, Woodcliff Lake, NJ 07677-7664. You may also fax your question to us at 201-690-5420 or e-mail it to memalp@advanstar.com
.





