Article
Practice Beat
Practice Parameters; Claims Processing; Managed Care; Fraud & Abuse; Complementary Medicine; Internet News.
Practice Beat
By Joan R. Rose, Senior Editor
Practice Parameters
Doctors sue over their link to "dangerous" guidelines
Two pediatric specialists in Texas are suing Seattle-based Milliman & Robertson, the publisher of clinical guidelines widely used by managed care plans to rein in costs and utilization. The suit calls into question the integrity of the company's pediatric guidelines and how they were put together.
In 1998, Thomas Cleary (a pediatric infectious disease specialist) and William Riley (a pediatric endocrinologist) were asked to review a prepublication draft of the company's newest guideline publication, Pediatric Health Status Improvement & Management December 1998. When the book was published, the doctors were listed among the "contributing authors"without their permission, they say. Cleary and Riley contend that the guidelines are flawed, and that they never approved them as "best practices."
In particular, the physicians take issue with the "goal length of stays," which they say have no basis in sound medical practice. Establishing goals for lengths of stay in a volume intended for use with children, they maintain, will result in "harm, injury, and death." By listing their names as contributors, the doctors' complaint argues, M&R implies that they endorse or recommend the publication, a suggestion that has damaged their professional reputations.
According to M&R's Web site, its guidelines are intended for use with uncomplicated cases and are "based on best observed practices throughout the country and on published research." But the company admits that the guidelines "aren't all based on controlled scientific studies"and asserts that "neither are the vast majority of current medical practices." Moreover, the company includes a disclaimer that the guidelines are merely suggestions and "not meant as a substitute for a physician's judgment about an individual patient."
Claims Processing
Upcoding vs downcoding (continued): Doctors and Humana come to terms . . .
After months of discussion, the Florida Medical Association and Humana have reached an agreement to ensure that physicians submit claims correctly and are reimbursed in a fair and timely manner.
Last summer, Humana instituted a new nationwide policy of reviewing all physicians' claims for coding accuracy. But physician backlash forced the managed care company to change its mind, and Humana now limits its review process to the fewer than 2 percent of doctors whose coding of level 4 and 5 claims is consistently higher than their peers'.
Under the new agreement, Humana will expedite its review process, and, together with the FMA, sponsor seminars to teach physicians and their staffs how to code correctly. The two also will meet periodically to assess the effectiveness of the agreement and the operation of the claims-coding initiative.
. . . as Medicare prepares to take a closer look at its third-party payers
The federal government wants to improve the accuracy and consistency of the private contractors who process and pay the nearly 1 billion Medicare claims filed each year. Beginning this summer, HCFA will review a statistically valid sample of each contractor's claims to determine whether health care providers were under- or overpaid.
Medicare will use the findings to establish contractor-specific baselines, which in turn will be used to measure future performance. The results, HCFA says, will reflect not only the contractor's performance, but also the billing practices of providers in the area.
The error-rate initiative will focus first on Medicare's four regional carriers for durable medical equipment and supplies, but HCFA expects to expand the program to all claims processors within a year.
Managed Care
Reimbursement policies: Do health plans consider quality of care?
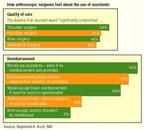
What doctors think is good clinical medicine is being curtailed by managed care rules. Nowhere is that more evident than in restrictions on paying for assistants in surgeryparticularly arthroscopic surgerysays Eureka, CA, orthopedic surgeon Raymond A. Koch. Managed care plans adhere to a less-is-more philosophy, while Koch believes that, where orthopedic surgery is concerned, less is less.
Though insurers, in denying payment, cite the opinion of their consultants, Koch says, "It's been my experience that the consultants they choose are handpicked more for their willingness to agree with the insurance company than for their expertise in the specific medical procedure they're evaluating."
To ascertain how widespread the use of assistants in surgery is, he surveyed members of The American Orthopaedic Society for Sports Medicine. Fifty-six percent of the 449 surgeons responding said they use an assistant (other than a scrub nurse) in more than three out of four arthroscopic surgery cases. Sixty-four percent prefer to have an arthroscopic assist on all procedures because they're unable to determine the degree of difficulty before going in.
Koch agrees with the majority who think insurers should allow full reimbursement if the operating surgeon believes that an assistant is needed to assure quality of care. But he concedes that a reduced payment should be considered in cases in which the operating surgeon "is unable to determine preoperatively whether an assistant is needed."
On a related issue, five other specialty societiesthe American Society of Anesthesiologists, the American Society of Cataract and Refractive Surgery, the American Association of Neurological Surgeons, the American Association of Ophthalmology, and the Congress of Neurological Surgeonsrecently sued the federal government over HCFA's refusal to reimburse physicians for the cost of clinical support personnel who assist at surgery.
Fraud and Abuse
Office space rentals: Uncle Sam's latest antikickback target
Some rental arrangements in which physician landlords lease office space to providers or entities to whom they refer may violate federal antikickback laws, warns HHS Inspector General June Gibbs Brown. In a special fraud alert, Brown addressed three features of these arrangements that are of particular concern:
- Appropriateness. Rental agreements should not include space that traditionally has been provided free or at a nominal charge for the benefit of patients. For instance, rental payments for consignment closets (for durable medical equipment) in physicians' offices would be suspect.
- Rental amounts. They should be at fair market value, fixed in advance, and not a reflection (directly or indirectly) of the volume or value of business generated between the parties. And if the space is sublet, the rent shouldn't exceed the rate paid by the physicians in the primary lease.
- Space and time considerations. The size of the premises rented should be reasonable and necessary for a commercial business purpose. Because it creates a presumption that kickbacks for referrals are disguised as rent, payments for space that exceeds the suppliers' needs would be suspect. The length of the lease would be suspect as well, particularly if it's too short, thereby allowing rental amounts to be modified (raised) more often than annually.
If you're currently involved in a rental arrangement or plan to enter into one, be sure that you comply with all six of the government's safe-harbor requirements for space rentals. To review the IG's special alert and the safe harbors, go to www.hhs.gov/oig/frdalrt/index.htm.
Complementary Medicine
Guess who's behind the latest push for integration
President Clinton has established a White House Commission on Complementary and Alternative Medicine Policy. Part of the Department of Health and Human Services, the commission will be charged with ensuring that all Americans have access to alternative disciplines.
The 15-member panel will recommend training for health care practitioners, coordinate research on CAM practices and products, provide health care practitioners with information that patients can readily understand, and offer guidance on when it's appropriate to use complementary and alternative disciplines.
Internet News
How do your health plans rate?
The National Committee for Quality Assurance has posted a Health Care Report Card on its Web site, www.ncqa.org, offering comprehensive information about the clinical performance, member satisfaction, access to care, and overall quality of more than 300 managed care plans around the US.
Plans are rated from zero to four stars in five key areasaccess/service, provider qualification, preventive care, getting better (how the plan helps people recover from illness), and living with illness (whether it has programs in place to assist patients with chronic diseases). The information is based on NCQA's Accreditation and HEDIS programs, and will be updated monthly.
NCQA has accredited about half the nation's 650 HMOs, and only those plans are listed in the database.
A new pathway to clinical trials
The National Institutes of Health has launched a consumer-friendly Web site offering easy access to medical research studies. The database contains information on 4,000-plus clinical trials under way at more than 47,000 locations nationwide.
Visitors to clinicaltrials.gov will find the design and purpose of each trial, where it's being conducted, criteria for participation, and the person responsible for recruiting participants. In many cases, further information about the disease and treatment under study is also available. No registration or personal information is required to use the site, so patient confidentiality is ensured.
The Web site grew out of 1997 legislation that required the Department of Health and Human Services to broaden public access to information "on drugs for serious or life-threatening diseases and conditions." Most of the trials currently listed are being run by NIH, but the database will be updated to include more trials from private industry and other federal agencies.
The database can also be accessed through the National Library of Medicine's Web site, www.nlm.nih.gov, and MEDLINEplus, medlineplus.gov.
Joan Rose. Practice Beat. Medical Economics 2000;8:24.





