Article
Practice Beat
Managed Care, Errors, Medicare, Medical Education, Access to Care
Practice Beat
Joan R. Rose
MANAGED CARE
Trouble in paradise: Doctors vs Hawaii's largest health plan
The Hawaii Medical Association is suing the state's largest health plan. The medical association contends that Blue Cross and Blue Shield (Hawaii Medical Services Association) deliberately underpays doctors by improperly downcoding, bundling, or refusing to accept codes with modifiers. In addition, the group charges that the health plan overrules doctors' "medical necessity" determinations without conducting a proper analysis or review, drags its feet when paying claims, and doesn't explain claim denials.
Physicians in Connecticut, New York, Tennessee, South Carolina, and New Jersey have filed similar lawsuits.
MEDICARE
Will PPOs revive Medicare's "plus choice" program?
Medicare will begin enrollment for a new coverage option next month. As part of a new demonstration program, 33 participating PPOs will offer a wider choice of providers than the program's closed-panel HMOs do.
The PPOs must offer all of Medicare's required benefits. Because they can require higher copays and deductibles, they'll also be able to offer greater benefits. HHS expects many beneficiaries to choose the PPO option as a way to obtain prescription drug coverage.
The pilot program will be available to about 11 million beneficiaries30 percent of all seniorsin all or parts of 23 states: Alabama, Arizona, California, Florida, Illinois, Indiana, Kansas, Kentucky, Louisiana, Maryland, Missouri, North Carolina, Nevada, New Jersey, New York, Ohio, Oregon, Pennsylvania, Rhode Island, Tennessee, Virginia, West Virginia, and Washington.
ERRORS
Message to docs: Get connected! STAT!
Small physician practices that rely on paper medical records are at particular risk for making medical errors. A study published in the British Medical Journal's Quality and Safety in Health Care examined medical mistakes in US primary care offices. It found that five out of six medical errors in family practices were administrative or "process" errors, like ordering the wrong test or prescribing the wrong medicationthe kinds of mistakes that electronic medical records and computerized clinical decision support systems are designed to prevent.
Of the offices studied, 73 percent did not have computerized medical records and 84 percent lacked Internet access.
MEDICAL EDUCATION
The diversity gap widens
The Association of American Medical Colleges says there's a growing "diversity gap" in the medical system. The number of minority students in US medical schools grew from fewer than 1,500 in 1990 to 2,340 in 1996. By 1999, however, the number had dropped to 1,912.
Also declining (by 46 percent since 1995): the number of graduates of medical schools abroad who are trying to get into US residency programs. One possible reason: The certifying exam now includes a clinical skills assessment, which costs $1,200, requires a trip to Philadelphia, and may be daunting to students who speak little English.
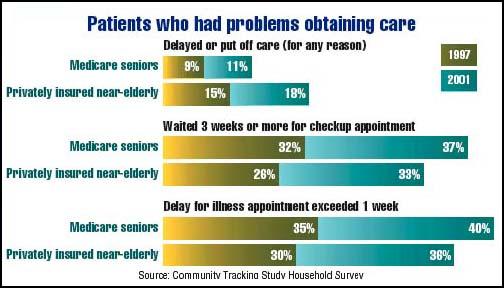
ACCESS TO CARE
It's not just a Medicare problem
Older patients are experiencing long waits for doctors' appointments, whether they're the privately insured near-elderly (age 50-64) or Medicare beneficiaries (65 and older). According to a study by the Center for Studying Health System Change, a nonpartisan policy research organization funded exclusively by The Robert Wood Johnson Foundation, the percentage of near-elderly who reported delaying or not getting needed care grew from 15 percent in 1997 to 18 percent last year. The proportion of underserved Medicare seniors rose from 9 to 11 percent.
The author is a Contributing Writer.
Joan Rose. Practice Beat. Medical Economics 2002;20:12.





