Article
Prior authorization made easier
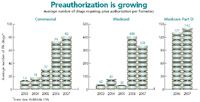
As more and more drugs require preauthorization, savvy physicians are finding ways to minimize the time and expense.

Key Points
Ask Frederic F. Porcase Jr., an FP in Jacksonville, FL, about prior authorization for prescription drugs, and you'll get an earful. The rules have gotten so complex and complying with them has become so onerous, he says, that "I now keep the $4 Wal-Mart formulary in all my exam rooms, because that's easier than anything else."
But you won't always find the appropriate generic drug to eliminate the need for insurance coverage. And if a new patient is already taking a brand-name drug for a chronic disease, the health plan's demands to justify its renewal can endanger the patient's health, Porcase says.
"Say a patient with a Medicare Advantage plan has been stable on Zyprexa, a very expensive but extremely effective psychiatric drug that most people take because they've failed on everything else. Now she comes here and wants a refill, but the Medicare plan will have this gauntlet you have to go through to get the refill through prior authorization."
Insurers counter that the goal of prior authorization or "step therapy" requirements is to cut the cost of health care and make prescription drugs more affordable for plan members. But even if that's true-and health plans aren't just trying to boost profits, as many physicians believe-prior authorization could increase practice costs because of the extra time it takes. Physicians and consultants say it can add five to10 hours of staff time per week in a small practice, and may require a medium-sized practice to hire an extra medical assistant.
Prior authorization also soaks up a lot of a physician's time. Aside from having to look through charts and fill out forms about a patient's medication history, doctors are often interrupted by nurses who want to know what to do about prescriptions that pharmacies have kicked back to them, notes Bay Shore, NY, consultant Michael Wiley.
Fortunately, there are ways to streamline your office processes to make Rx preapproval less painful and time-consuming. Here are some methods that physicians and practice management consultants suggest to lighten the load.
Forms and formularies keep changing
Keeping forms and formulary lists close at hand, using a combination of experience and gut instinct to figure out which nongeneric drugs can be safely prescribed without prior authorization, and asking drug company detailers for information about coverage are among the strategies doctors are trying.
To reduce the amount of phone time spent on hold with health plans, FP Craig Wax of Mullica Hill, NJ, has his staff pull down prior authorization forms from web portals that some insurers and pharmacy benefit managers (PBMs) use to facilitate transactions. When PBMs fax such forms to his office, he keeps copies so he'll know when a particular payer is likely to require prior authorization.
Wax's approach helps but has its limits. Because preapproval is required for so many medications, and because both the drugs and the questions about them vary among plans, it's almost impossible to keep track of all these forms.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.





