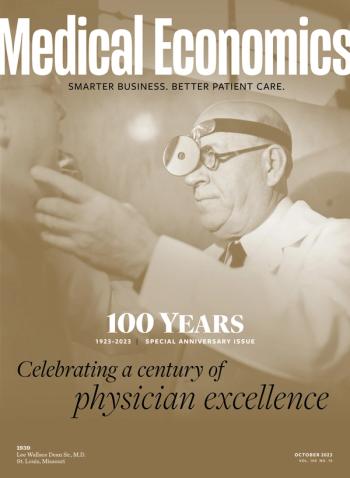
- Medical Economics October 2023
- Volume 100
- Issue 10
How modern medicine was made, part 3: The history of antibiotic development
'From weird and wonderful places'
Physicians of the 1920s likely had heard of Paul Ehrlich, the Nobel Prize-winning German doctor who developed arsphenamine, known by the brand name Salvarsan. In the 1910s, it was the first antibiotic drug to cure syphilis, and Ehrlich now is regarded as a father of chemotherapy.
But it would be the 1930s when new sulfa drugs “revolutionized medicine,” according to the National Institutes of Health. In 1935, German physician Gerhard Domagk published his findings about Prontosil, the first sulfonamide drug. Human test patients included his 6-year-old daughter, who contracted a severe streptococcal infection but fully recovered with the new medicine. Scientific and public interest took off, setting the stage for further research — and modern drug regulation.
In 1937, a Tennessee company marketed “Elixir Sulfanilamide” for parents to treat streptococcal infections in their children. It was a “therapeutic disaster,” an “untested product … a highly toxic chemical analogue of antifreeze,” that fatally poisoned more than 100 people, including many children, according to the official history of the Food and Drug Administration (FDA). Public outrage spurred lawmakers to pass the U.S. Food, Drug, and Cosmetic Act of 1938, landmark legislation requiring drugmakers to get government approval before selling new medicines to the public.
Although tragic, those deaths did not stifle medical and public interest in new cures.
Another began brewing in 1928, when Scottish professor of bacteriology Alexander Fleming found a penicillium mold had contaminated and killed one of his bacterial cultures. Cultivating it, Fleming found it wiped out many kinds of bacteria but was harmless to mice that were injected with it. In 1929, Fleming published his findings with “only a passing reference to penicillin’s potential therapeutic benefits,” according to the American Chemical Society (ACS).
It would be another decade before physician Howard Florey, biochemist Ernst Chain and their colleagues at Oxford University’s Sir William Dunn School of Pathology “turned penicillin from a laboratory curiosity to a lifesaving drug,” according to ACS.
On Feb. 12, 1941, Albert Alexander, a 43-year-old police officer, became the first patient to use Oxford penicillin to fight a life-threatening infection that developed from a scratch on the side of his mouth while pruning roses. Alexander began recovering, but the supply of the drug ran out and the infection claimed his life.
As World War II raged, research moved to the United States in hopes of purifying and boosting production of a wonder drug that could help the Allies, and it worked. At the same time, microbiologist Selman Waksman, working in New Jersey, led the team that discovered new antibiotics and in 1943 isolated streptomycin, the first antibiotic effective against tuberculosis.
In 1945, Fleming, Chain and Florey shared a Nobel Prize for their discoveries. Waksman received his in 1952. And patients were asking their doctors about penicillin.
With peace restored, drug companies began collecting soil microbes “from weird and wonderful places” in the quest to find more natural products of bacteria, mold and fungi to become new antibiotics, says Matt Hutchings, coauthor of a history of antibiotics and head of molecular biology at The John Innes Centre, an independent firm in Norwich, England, that researches plant science, genetics and microbiology.
“Almost all the drugs we still use are derived from molecules discovered during this time,” says Hutchings, who described the 1940s to the 1960s as the golden age of antibiotics.
The postwar antibiotics boom revolutionized medicine, says David Hyun, M.D., director of the Antibiotic Resistance Project for the Pew Charitable Trusts.
“Antibiotics really changed the course of how we can act, the effectiveness of the health care that we provide, and that goes beyond treating patients with infections,” Hyun says. “It underpins the success of chemotherapy patients, treating patients with cancer. It underpins the success of surgical procedures.”
Discovery eventually gave way to rediscovery, finding the same natural products or properties repeatedly, so research slowed, Hutchings says.
In the 1930s, Fleming hoped to inspire experimentation, so he sent samples of the mold to about anyone who asked. Now it costs drug companies a lot of time and money to find new antibiotics, test them, get required approvals and get them to market, the experts says.
Drugs are valued by volume of sales, Hyun says. The market produces lifetime drugs to control conditions like cholesterol levels and hypertension, but antibiotics are a short-term therapy.
“Most of us take antibiotics for just for a single infection, and chances are if you’re a healthy individual, without any other chronic conditions — that’s it, you won’t have to take the antibiotic again, maybe for the rest of your life in some situations,” Hyun says.
For decades, people were not the only ones using them. Antibiotics were added to poultry and livestock feed to aid in weight gain, to plant sprays and food preservatives, and by the 1960s were spreading across global food production.
In his Nobel Prize lecture, Fleming described specifically how bacteria could build resistance to penicillin through exposure to small doses. That is exactly what is happening with various bacteria and antibiotics on a global scale.
“Resistance was observed nearly from the beginning. It was largely ignored,” says James E. Kirby, M.D., professor of pathology at Harvard Medical School and principal investigator in the Experimental Pathology Division of Beth Israel Deaconess Medical Center in Boston. “We were finding so many new antibiotics and we had solutions for essentially everyone.”
By 2017, the World Health Organization could declare: “The world is running out of antibiotics,” with antimicrobial resistance “one of the biggest threats to global health, food security and development today.”
Kirby called the problem “insidious and incremental.” Hutchings says “the best and most horrifying” example is multidrug-resistant and extensively drug-resistant tuberculosis. He also pointed to a study that estimated 1.2 million people died from drug-resistant infections in 2019.
“Once we started losing the effectiveness of the antibiotics, all those medical advances that we have achieved in the last century, we’re jeopardizing the successes and the advancements that we have made in saving lives,” Hyun says.
But, again, new discoveries await, and maybe some rediscoveries. This spring, Kirby’s team of researchers learned nourseothricin, a natural product made by a soil fungus, could be effective in killing bacteria resistant to other antibiotics. Nourseothricin was discovered in 1942, abandoned due to toxic effects to the kidneys, but refined and revisited for 2023.
Nature may hold more, especially aquatic environments not yet fully explored. “I believe there are a lot of antibiotics produced by our environment microbes,” Kirby says. “We just have to be cleverer in finding them.”
How modern medicine was made: Table of contents
Introduction Part 1: The importance of medical imaging Part 2: The power of vaccination Part 3: The history of antibiotic development Part 4: The importance of insulin's discovery Part 5: The development of surgery and organ transplantation Part 6: Military medicine advances health care for soldiers and civilians Conclusion: Improving lives
Articles in this issue
over 2 years ago
The future of medicine - what patients expectover 2 years ago
The doctors bag in 2023over 2 years ago
The doctor's bag in 1923over 2 years ago
A century of primary care transformationNewsletter
Stay informed and empowered with Medical Economics enewsletter, delivering expert insights, financial strategies, practice management tips and technology trends — tailored for today’s physicians.