
At-risk students and diversity both suffer from changing the first part of the exam to pass/fail
Todd Shryock is managing editor of Medical Economics.

At-risk students and diversity both suffer from changing the first part of the exam to pass/fail

Different generations face different problems when it comes to accessing health care.

Growth is still anticipated for many, despite challenges


Decreasing volumes and bad debt take a toll

Costs expected to exceed more than $15,000 per employee
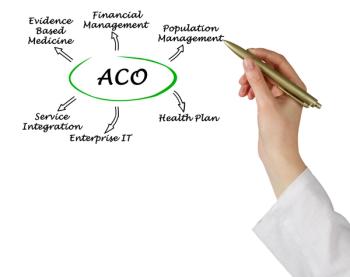
63% of ACOs earned shared savings in the program

Russian-based hacker group responsible for much of the activity
Insurance giant says it will remove prior auths for 25% of medical services

Most patients don’t have a specific ownership preference, but those that do overwhelming prefer independent private practices

AI shows how it can increase accuracy in clinical care and assist doctors with decision-making in the future

The latest health care technology news

Study examined more than three million ED visits

Survey shows that patients want a lot more from their health plan than what they are getting

15-plus insulin and diabetes care brands are covered


ProPublica report illustrates the influence that a single lobbyist can have on CMS policy decisions that take billions away from doctors and redirects it to insurance companies.

Data analysis by the paper showed an average physician salary of $350,000

Company exiting three states and Puerto Rico this year, warns of cash shortfall
Survey shows that health care execs think generative AI will solve many of the industry’s problems, but aren’t doing much to adopt it

Patients have limits as to what they are willing to give up in order to secure the long-term sustainability of Medicare


Even with the pandemic no long dominating their lives, both doctors and their patients struggle with stress

Provider productivity rises despite financial pressures

The latest health care and technology news

Survey shows how little faith patients have in technology – and the companies that provide it -- to protect their information

Survey sheds light on how patients are feeling about billing, privacy, and other health care-related issues.

Central bank increases interest rate for the 11th time since March 2022


Health care continues to lead all sectors with the most expensive data breaches