Article
Practice Beat
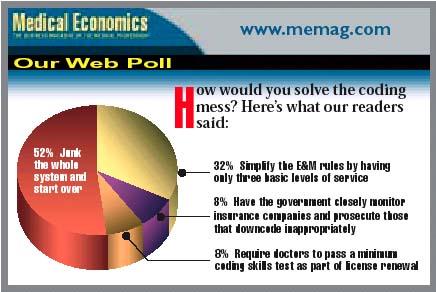
Boutique Medicine, Reimbursement, Allied Health, Collective Bargaining, Our Web Poll
Practice Beat
Joan R. Rose
Boutique Medicine: Will Congress halt the move from health care to wealth care?
The growing trend toward "concierge medicine"medical practices that offer personalized services for an extra feehas caught Congress' attention. Earlier this year, Rep. Henry Waxman (D-CA) and four other congressmen wrote to HHS Secretary Tommy Thompson and HHS Inspector General Janet Rehnquist urging them to send a clear message to such doctors that they must opt out of Medicare.
The congressmen say that requiring an additional fee as a condition of providing Medicare services means that the patient is paying for the opportunity to receive covered benefits, even if the money supposedly goes for noncovered services. And if the doctors bill Medicare for those services, they're not only violating the law that limits patients' charges, they're violating fraud and abuse laws.
Congress is also considering legislation that would specifically prohibit doctors who charge access fees from billing Medicare for their services.
Collective Bargaining: Alaska tries to level the playing field for physicians in the Last Frontier
As a national physician antitrust bill continues to languish, Alaska is the latest state to move forward to clear negotiation hurdles for providers. That state's Senate passed a billby a two-to-one marginthat would allow competing physicians to collectively bargain whenever a health plan's market power would otherwise enable it to dictate the terms of the contracts it offers doctors.
The measure, which awaits House action, would allow collective bargaining on fee-related and other issues, including clinical practice guidelines, coverage criteria, and liability for treatment decisions. Off-limits during negotiations: issues involving the exclusion of nonphysician providers from direct reimbursement and the settings in which they render services. The bill, which in many respects resembles those enacted in Texas and Washington state, also limits the size of the bargaining group and prohibits physicians from engaging in an express or implied threat of retaliatory action.
Reimbursement: No more secret fee schedules, this court tells insurers
Issuing a final judgment in a landmark suit, a Georgia trial court has ordered Blue Cross and Blue Shield of Georgia to disclose its fee schedules and reimbursement methodology to participating physicians. In addition, the court said, any promise of future compensation that isn't stated as an exact amount must be readily discernible by physicians using information provided by the plan.
The suit pitted the Medical Association of Georgia against the giant health plan. Doctors contended that BCBS had improperly modified its definition of uniform, customary, and reasonable charges. Earlier, an appeals court had said that although BCBS had the right to change its fee reimbursement program, the insurer couldn't refuse to provide physicians with a fee schedule and the formula used to determine it. The state Supreme Court agreed, and sent the case back for trial. When the state medical association and the Blues couldn't agree on how the ruling should be implemented, the trial court delineated the terms and gave the insurer 30 days to comply.
Allied Health: Minnesota CRNAs will practice autonomously
Minnesota has become the fourth stateafter Iowa, Nebraska, and Idahoto opt out of a controversial Medicare rule that requires certified registered nurse anesthetists to be supervised by physicians.
Doctors long have fought to retain the requirement and, late last year, the Centers for Medicare & Medicaid Services agreedbut left states some wiggle room. A governor can override the requirement if, after consultation with the state medical and nursing boards, it's determined that access to care would otherwise suffer.
The author is a Contributing Writer.
Joan Rose. Practice Beat. Medical Economics 2002;12:14.





