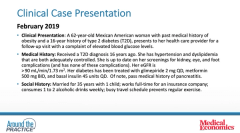
Analysis of Type 2 Diabetes Mellitus case by expert panel
Episodes in this series

Stephen A. Brunton, MD, FAAFP: There are a number of issues. If you have a patient who’s uncontrolled like that, ask them what’s going on. She’s saying she’s been forgetting it. What is it that we can change about her lifestyle, so that this isn’t happening? The other thing I’d want to know about is hypoglycemia, which we talked about before. You sometimes have reactivation. She’s getting low, so she’s eating more to compensate for that, and that can often result in untoward A1C [glycated hemoglobin] levels. She’s on a sulfonylurea, and we talked about how that makes it more likely that she is going to have hypoglycemia, so I’d be thinking about that.
The other thing is this: I’d try to maximize the metformin. She’s on once a day, but I would like to get it maximized to twice a day. The issue is then talking about some of the adherence issues she’s having anyway. What is it about her lifestyle that’s creating that? She would be an appropriate person to consider working with a diabetes educator; she needs to see a diabetes educator. If not, she needs to be, because it may be about food choice as well. As I mentioned, I work with a large Mexican American population, and I work with 2 Hispanic PAs [physician assistants], and they call it tortilla poisoning, because it’s really about dietary choices. We have to develop a diet that’s going to work with them, so a dietitian will be good, as will working with a diabetes educator to maximize the lifestyle issues. I then think that, now that Diana is working in my practice [Primary Care Metabolic Group], she can be discussing with that person the potential appropriateness of an insulin pump.
Robert Busch, MD: Before we get to Diana as the pump guru, the patient had pancreatitis, so that was in the case because it throws out our good classes of drugs: GLP or DPP4. What was the cause of her pancreatitis? Did she have her gallbladder out and there were gall stones? Did she drink alcohol, but now she doesn’t drink anymore? Were her triglycerides way high but are now at a normal level? Even though the GLP class has not been studied with pancreatitis, I see many of us who, if a patient had a cause of their pancreatitis that is no longer there, have used GLP cautiously in those patients as well as cleaning up diet, exercise, and all that.
She hasn’t been on SGLT2. You’re not going to get her to goal just by adding an SGLT2 when she’s in the 9%, and she’s already on insulin, but that may help. She has hypertension, and she’s obese, so that’s something I would use unless she’s had 10 yeast infections and comes to me on an antibiotic and has a yeast infection. We still have some other stuff we could do. I don’t know if I’m going to jump in with a glitazone because she’s already overweight, unless her triglycerides are way high. She’ll need some tuning up of her diabetes and lifestyle, and all that would be very important.
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: Yeah.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: That’s an excellent point regarding the guidelines and what we talked about. Here, we’re assuming that the patient is on basal bolus insulin, but for the point you made about the SGLT2, we’re digging more to see if there is a reason for some of the points that you highlighted. On a first glance, the patient’s EGFR [estimated glomerular filtration rate] seems fine, which is sometimes a reason our patients are excluded, but that’s certainly a great point. Diana?
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: I would want to explore more about missing the insulin doses. I completely agree with the medication adjustment or evaluating the other medications as well as the referral for a dietitian and diabetes care and education specialist. I also want to make sure she has the right understanding and expectations about an insulin pump. An insulin pump could certainly be a good option, but some people have these false ideas about it that aren’t necessarily true. One of them could be that it’s set. You just put the thing on or have it surgically implanted, then you don’t do anything for your diabetes anymore. We want to make sure she understands what an insulin pump is and that she would still need bolus insulin for meals and stuff. I would want to explore more about what the reason is for not bolus insulin dosing to make sure a pump is going to be the right fit.
Stephen A. Brunton, MD, FAAFP: She may have some concerns about insulin. I see that a lot in my patient population: They agree to go on it, but they try to minimize using it as much as possible. With her on triple bolus insulin therapy as well, something doesn’t fit, and we need to penetrate further into what some of her considerations might be.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: Let’s unpack that. When we’re talking about reasons for patients who are on multiple daily injections, what are some things that you see with someone who is not reaching their A1C goal? Diana, if you have them on a CGM [continuous glucose monitor], and you’re not happy with their time and range, what are some things that you’re seeing or things you’re suspecting?
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: One big thing that we see is the inconvenience of taking the insulin. That’s a huge barrier. Some people take just their basal insulin as their prescribed 3 mealtime injections a day and then go many days without taking that. For inconvenience, that can be a great thing. With CGM, what we see in those situations is that there are large postprandial glucose spikes. As we were talking about earlier, some of these patients are overbasalized, so what you see is there are these big drops. Sometimes there’s hypoglycemia, and sometimes it’s going to bed at 350 mg/dL and waking up at 100 mg/dL, but you see you’re stuck. You can’t go up any more on the basal insulin, but there is large hyperglycemia happening at mealtimes or anytime they’re eating a meal or snack. It’s clear that they need those bolus insulin injections.
Stephen A. Brunton, MD, FAAFP: This is really where the CGM, particularly flash glucose monitoring, is a game changer for us as clinicians to review their profiles but also for patients to be educated about what they’re doing in their lifestyle, particularly diet, that’s causing those elevations. If they’re measuring their blood sugar, a lot of patients do a basal glucose measure, and that’s it. But being able to do that, monitor it, and see what they’re doing provides some unique opportunities, particularly if they’re also keeping a diary. You can see it, and you can work with the patient in terms of counseling them on what can be done differently. That in itself will often get a patient back to normal mostly.
Robert Busch, MD: That’s right. If she went to an educator, cleaned up her diet, and had a CGM on to see what the different foods are doing, that can have a dramatic effect on her A1C and normalizing her blood sugar by maybe taking enough basal and eating properly. She can jump-start her pancreas by taking away glucose toxicity, and maybe her other pills will work better.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: Absolutely. We know that the behavior changes and lifestyle changes with any kind of condition, specifically with diabetes, can have a tremendous impact. Those are certainly things we should suggest.
Newsletter
Stay informed and empowered with Medical Economics enewsletter, delivering expert insights, financial strategies, practice management tips and technology trends — tailored for today’s physicians.