Clinical Case Presentation
Episodes in this series

Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: We’ve talked a lot about all the different things, starting with the pathophysiology. We talked about diagnostic criteria, the guidelines, and all this new innovation that we’re seeing in diabetes technology. We have smart insulin pens, we have CGMs [continuous glucose monitors], and we have insulin pumps. How do you then put all this into practice? What I want to do is take some time and present a patient case, and I want everyone to take a few minutes to digest it. If this was a patient who was in your clinic or was presented to you, I’d love some initial feedback on what you’re thinking, whom you might refer to, and your thought process.
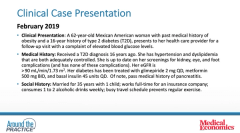
The patient we’re talking about here is a 62-year-old Mexican American woman who has a past medical history of obesity, a 16-year history of type 2 diabetes. She presents for a follow-up visit with a complaint of elevated blood glucose levels.
Her medical history is this: As I mentioned, she has had type 2 diabetes for a significant amount of time, 15 to 16 years. She’s also had hypertension and dyslipidemia. Luckily, those are both adequately controlled at the moment. She is mindful of her complications. She’s getting her screenings done on a regular basis: eye exams, foot exams, and kidney screenings. Her EGFR [estimated glomerular filtration rate] is under a good number right now: it’s greater than 90 mL/min. Her diabetes is currently being treated by a sulfonylurea, so she’s on glimepiride 2 mg once a day, metformin 500 mg twice a day, and 45 units of basal insulin. She also has a past medical history of pancreatitis.
A bit about her: She is married with 1 child. She works full time for an insurance company. She consumes maybe 1 to 2 alcoholic drinks a week, but she has a hectic schedule, and it prevents her from regular exercise.
I’ll give you all a bit about the physical exam as well as some of the pertinent labs. The patient is overweight with a BMI [body mass index] of 35 and an A1C [glycated hemoglobin] level of 9.2%, and this was in February 2019. Fasting blood glucose at the time was about 180 mg/dL.
A bit about her medications and the current therapy she’s on: She’s covered with a statin. She’s got an ACE inhibitor on board from a diabetes medication standpoint. As I mentioned, she is on 500 mg twice a day of metformin, 2 mg of glimepiride, and 45 units of basal insulin. She takes a multivitamin. Once she was started on that basal insulin, she was eventually added and titrated onto bolus insulin, so she is on 15 units of bolus insulin 3 times a day.
If you fast-forward, you’ve had this patient who’s on multiple daily injections, and her A1C has improved from what it used to be after the addition of the bolus insulin; it’s sitting at 8.7%. She’s feeling well. Her A1C has improved a bit, but she tells you she’s missing bolus insulin doses quite often. She takes them later because her schedule is hectic. She comes in and says, “What can you do to help me with this? I want to do better. Is there something that I can do?” She asks, “What about an insulin pump?”
Newsletter
Stay informed and empowered with Medical Economics enewsletter, delivering expert insights, financial strategies, practice management tips and technology trends — tailored for today’s physicians.