Considering a Continuous Glucose Monitor
Episodes in this series

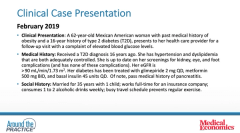
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: Let’s say we’ve done those. We’ve had some success, probably not to an A1C [glycated hemoglobin] level that Bob is going to have with his patients, but we still need to go. The patient now needs an insulin pump. Diana, what’s coming to mind about where you might go or what tool you would pull out of the toolbox as you consider selecting an insulin pump? We’ve gone through the checklist, and this is the ideal candidate, so what are you thinking here? What may be some of the features that are most important not only to you but to your patients as well? In this case, it’s this 62-year-old patient sitting in front of you or with whom you’re virtually engaging.
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: I’ve got demonstration models at my site [Cleveland Clinic Diabetes Center], and I love to break everything out and show people. They can put their hands on it, see what the menus are like, and play around with it. They even understand that if they are going to use it to take bolus insulin doses, what that looks like. I’m pulling out what the infusion sets look like, and they can see where it would go on their body. They see what the size of it is, and they see it and feel it for themselves to see to see how they like it. For a lot of people, it’s smaller than they realized. The idea is that you usually have to change it out every 3 days, which is a lot easier than having to do something daily or multiple times a day.
With all those things, I would share that information, but I’d also share about some of the other expectations, such as how, every 3 days, you still need to fill it up with insulin and that, when you’re getting ready to eat, you need to enter in either your carbohydrates or the decided meal estimate. Ideally, with our current insulins and how they work, it is ideal to pre–bolus insulin dose before you eat, so there is still that education.
One of the nice things with pumps is that you can also set reminders. If a person forgot to take a bolus insulin dose, you can set an alarm to remind them to do it at certain times of the day. One of the features I like is when we have that CGM [continuous glucose monitor] integration. Before, we talked about the Medtronic 630G and how that is integrated with the Guardian Sensor to be able to suspend insulin. A lot of people have their fear of hypoglycemia. That is something I would explore with her because that is sometimes a barrier to taking the insulin.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: Sure.
Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES: It may be that those 15 units are too much. Maybe she’s given herself the 15, and she dropped really low, so she’s now worried about doing that. That’s where a feature like that could really be beneficial.
Dhiren Patel, PharmD, CDE, BC-ADM, BCACP: Yes. That’s an excellent point. With all this technology, there are different features, and you just highlighted some for the 630G that make it attractive for this specific patient. Whether it’s the 630G from an insulin pump standpoint or even introducing the InPen, the message is this: Let’s figure out what those barriers are because we need to do a better job. Steve, you mentioned this at the beginning. There are a lot of red flags here. Let’s unpack as many of them as we can before we assume and impose our bias and say, “Here’s what you need.” Bob, you mentioned getting some of that basic stuff. She may have not had that lifestyle education or the educator’s help. Let’s try to do that. Diana, what I’ve heard from you is that there are a lot of options, but let’s figure out what technology is going to work best for this patient.
This has been an excellent discussion, and we hope you found this information helpful. I want to thank you all for your time and for providing your excellent expertise. We appreciate all of you watching this Medical Economics® Around the Practice program. Thank you.
Newsletter
Stay informed and empowered with Medical Economics enewsletter, delivering expert insights, financial strategies, practice management tips and technology trends — tailored for today’s physicians.