
If the choice of personal medical care offered by small practices is to be preserved, the rules of the game must change.

If the choice of personal medical care offered by small practices is to be preserved, the rules of the game must change.

Here’s a look at what 2019 may hold in four areas of healthcare policy of importance to doctors: the future of the Affordable Care Act, expanding healthcare insurance coverage, the cost of prescription drugs and changes to accountable care organizations.

The free market would provide abundant care.
Here are the reimbursement trends physicians can expect in 2019.

A new bill recently introduced to Congress would not only reduce barriers to genetic counseling for Medicare patients, but also could significantly decrease costs of caring for elderly and low-income patients.

For many in healthcare, words and actions can be harmful, and in some instances can lead to jury awards in the hundreds of thousands of dollars.

There is a patient safety organization for practices of every type and size, and nearly all healthcare providers have important interests that can be served that are well worth the costs.

Four physicians allege ABIM is illegally tying its initial certification to MOC.

Consent is a controversial subject and has significant ramifications in the healthcare delivery system.

Government regulations ranks 3rd on the list of issues ruining medicine for physicians.

An American solution focusing on individuality and conserving resources can save the Medicare program.

Nothing is set in stone, but healthcare compliance leaders should start preparing for the following three changes.

Should physicians have a voice in the ongoing debate about gun control? The National Rifle Association doesn’t think so.

Quality Payment Program and Physician Fee Schedule both see changes

Special interests keep patients in the dark, right where hospitals want them.

When complicated medical-related legal issues arise, physicians are often asked to provide expert opinions.

The Trump administration insists rebates cause inflated prices, but what would it mean to physicians and patients if the system ended?

Pharmacy chains purchasing payers will alter the healthcare landscape.

As businesspeople, providers must understand the risks involved in providing telehealth services in other states.

When it comes to telemedicine services, the primary factor affecting reimbursements is legal policy.

Despite the benefits of telehealth to consumers, laws designed to protect state healthcare providers and patients often stand in the way.

The proposed new rule would make it harder for accountable care organizations to realize the financial benefits of participating in the Medicare Shared Savings Program without also taking on more financial risk.

Because CMS can’t and Congress won’t get rid of hospital-based facility fees, doctors and patients must take action.

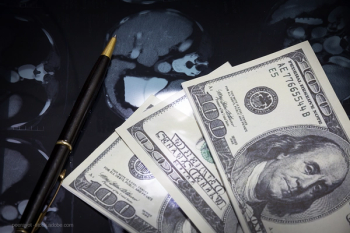
In the value-based payment era, the opportunity for greater financial rewards comes with greater risks.

While CMS says it aims to allow doctors more time with patients with less documentation, its proposed E/M changes simply don’t achieve that goal.